Cause for optimism in healthcare?
It's time to build healthcare products that cost less, and improve patient health outcomes
Did you know that 66.5% of all bankruptcies in the US were tied to medical issues (either because of high costs for care or time out of work)?
On a personal level I was thinking about my interactions with the system over the past 10 or so years. In that time I’ve navigated a cancer diagnosis, diagnosed a son with ADHD/Autism and all the ancillary support systems, helped family work through many (some severe) mental health challenges, wrangled more financial claims than I can count, seen chronic diseases, shopped for wheelchairs and accessibility vans for my mother-in-law, and worked through genetic screens, and births for 3 children. I’ve been fortunate to live in urban environments close to centers of excellence. And I’ve had the means to pay out of pocket for additional support when it was needed. And still the variance in quality and preventable issues/errors has been unacceptably high.
That got me curious about the larger state of things. In evaluating the state of the US healthcare system here’s a few high level points I’ve found helpful:
US costs are increasing, and household expenditures reflect this trend:
The US spends more on healthcare than any other high-income country. In 2021, health spending in the US exceeded $4 trillion (18.3% of 2021 GDP). This is double what other developed nations spend - and for generally worse outcomes.
The chart below does a great job summing up our purchasing power along various goods and services. Notice that degree to which hospital and medical care services have outpaced other costs, including hourly wages! As a percentage of family income our healthcare expenses have steadily increased since the 1950s: from about 5% in the 1950 to ~15-20% in the 2020s. Over 20% of Americans have medical bill problems or are paying off medical debt.
Doctors hate the system
The stats I’ve seen indicate burnout is a real issue. Much of this has to do with the arcane technologies they use daily - specifically the electronic medical systems. These are systems that are expensive to maintain, prohibitively expensive to switch out, and in which the builders themselves have little incentive to innovate. And it seems this trend may be impacting med school enrollment with applications trending downward. The Doctors I know went to med school to make a difference, not to be glorified pharmaceutical pushers and coding monkeys (taken from actual conversations).
Patients don’t trust the system….and for good reason
Fewer than half of Americans have confidence in the medical system - in 1966 this number was 76% and fell to 34% in 2018 (Gallup, 2021). Who could blame them?
Medical errors are a leading cause of death in the US, with estimates ranging from 250,000 to 440,000 deaths per year due to preventable medical errors. It’s hard to say what part of this stems from the clear lack of a unified health record system which clearly leads to fragmented care, with different providers not having full access to a patient's records. In 2020, the US infant mortality rate was 5.4 deaths per 1,000 live births, while many European countries have rates below 3.5.
Well-intentioned Providers are as blind men feeling the elephant that is a patient’s medical history.
From a cost perspective, the same procedure can have widely varying costs between different hospitals or even within the same hospital. Surprise medical bills are a common issue, with patients receiving unexpected charges for out-of-network services even at in-network facilities. Beyond this, the so called fee-for-services model incentivizes unnecessary medical tests and treatments that strike the wrong balance between patient harm vs. litigation protection.
So that’s the current state of things - not great.
But there’s cause for optimism
This optimism is not so much due to any regulatory shifts or governmental innovations, so much as a summing of large forces spanning a range of technologies.
And it’s the output of this effect that will fundamentally alter the relationship patients have to the healthcare system. Or, if you liked the documentary the hundred-foot wave, you can think of it like the set of forces leading to those monster waves in Nazare: shelf dynamics that lead to wave speed shifts, steep depth reduction, waves convergence from two directions, and local water channels. I suspect the coming decade will produce some magical collissions
To that end here’s a - definitely non-exhaustive - set of forces that are very much in-play, but haven’t broken into the practice of medicine or healthcare delivery in real ways.
Life science innovation will accelerate
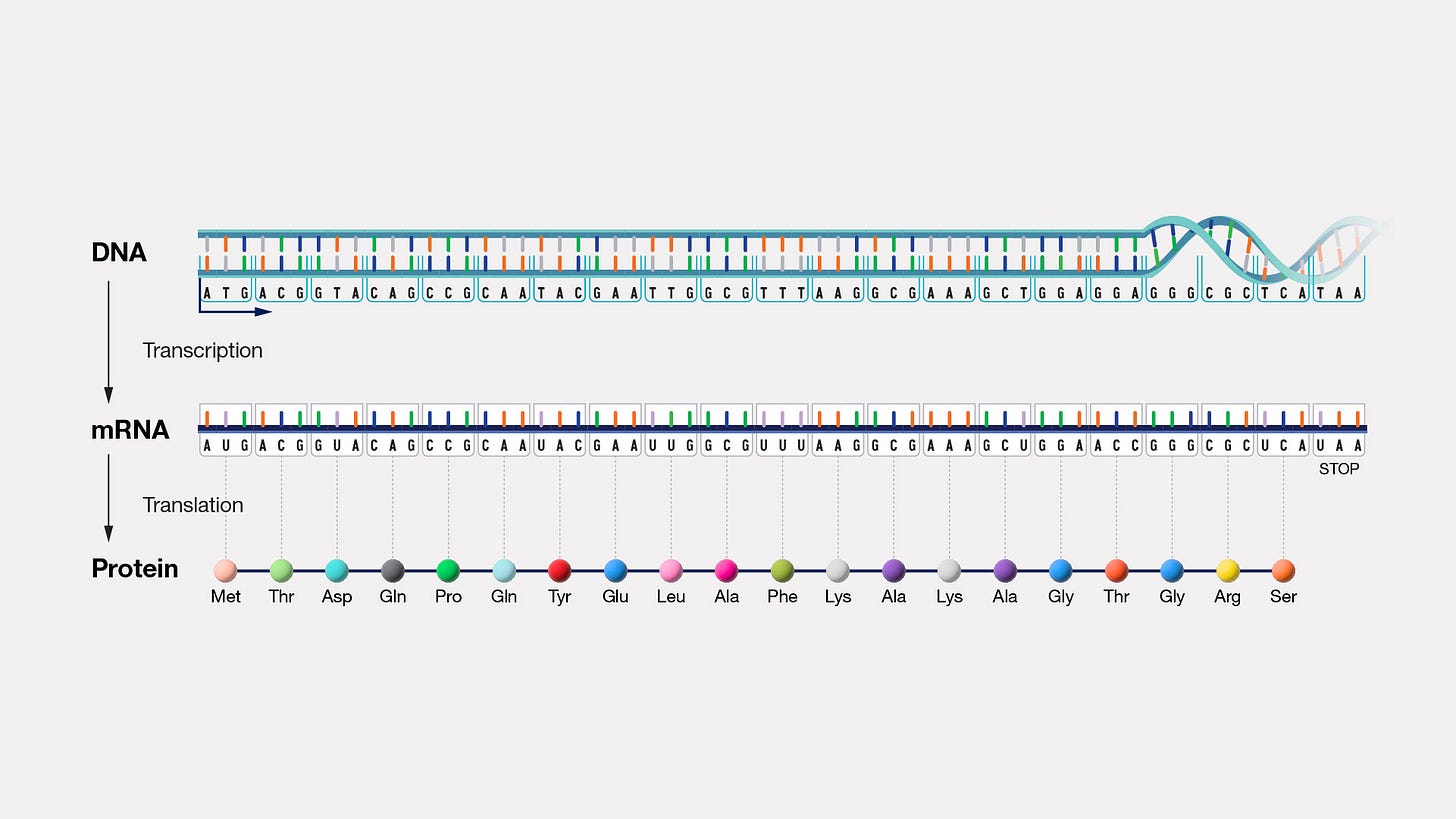
A good way to think about life sciences is through the lens of the so-called “central dogma”. This roughly says that DNA encodes RNA, which encodes Proteins. In this story DNA is the blueprint that ultimately builds the functional biological units and systems through Proteins. We’re seeing innovations at all levels of this “stack”.
For example:
CRISPR is a technology most of us have heard about - typically called gene-editing tools. This, and other related technologies are giving us read/write access to the human genome in ways that are both jaw-dropping and concerning, in the brave-new-world/designer babies sense. But this is a new frontier that will change things for us. Along these lines the CRISPR gene-editing market is expected to grow from under $2b billion in 2022 to $15b by 2030. And that’s something considering the costs of genomic sequencing have outpaced Moore’s law (the well known trend in which computational costs half every ~18mo) for over a decade. This trend has brought costs down by a factor of 10 in the past decade, to below $1k for a human genome.
At the protein level DeepMind's AlphaFold has predicted structures for nearly all catalogued proteins known to science, over 200 million structures (Nature, 2022). This is astonishing. I’m not that old but when I was working at UCSF I knew post-doctoral fellows who would spend literally years trying to isolate a mere snapshot of a protein’s structure using non-computational methods like crystallography. Given that proteins are the primary functional units of biology I’d expect this will massively accelerate research progress, drug discovery and treatments.
AI and LLMs
I was talking with a researcher the other day who told me about a 2022 study that showed GPT-3 performed at or near passing level on the United States Medical Licensing Examination (USMLE) without any specialized training. This ~2 year old technology is on par with Harvard or Stanford medical students! And AI systems have shown comparable performance to radiologists in detecting breast cancer in mammograms (Nature, 2020).
Data/Consumer wearables
Telemedicine usage increased from 11% of US consumers in 2019 to 46% in 2020 due to the COVID-19 pandemic (McKinsey, 2021). This level is still sustained and, moreover, consumers now expect this. It’ll be hard to go backwards from these levels.
Consumer devices and digital health is expected to grow 15% (CAGR) from 2023-2030, from $200b today, to over $650b by 20230. This includes everything from home monitoring e.g., smart scales, to watches to apps etc. We should expect this data to start making it’s way into medical practice. Most patients consider it important to be able to access their health data easily.
Other technological innovations/Science fiction bucket
No update would be complete without admitting that from here we can only see so far into the fog. But there’s magic inside. Just yesterday the Neuralink group reported on progress on brain-computer interfaces. This is actually not a new technology, per-se (it was originally called Brain Gate out of Brown U.). But if Elon is working on a technology there’s good reason to believe progress will manifest.
Where do we go from here?
The amount of white-space in this field ought to whet the appetite builders interested in improving the sorry state of the US healthcare system. While I don’t have a crystal ball, I’ll bet there exists an opportunity inside of patient self-serve models focused on at three specific aims:
Improved outcomes (e.g., improved access to quality care, engagement, identification of high risk/needs populations)
Reduce overall costs - opportunity exists for both patients and for hospitals/providers/employers (e.g., via self-serve tools for patients, better claims management, avoiding unnecessary procedures, getting quality PCPs).
Increase engagement (e.g., remote patient monitoring, wearable/consumer tools, habit changes).
My hope is that a set of Entrepreneurs, Innovators, Scientists and Clinicians & Care Givers will leverage these forces to bring needed innovation to the industry.
Are you working on something in this space? I’d love to hear about it!
Sources
https://www.nature.com/articles/d41586-022-02083-2
https://www.statista.com/topics/8219/medical-debt-in-the-us/#editorsPicks
https://www.grandviewresearch.com/industry-analysis/crispr-associated-cas-genes-market
https://www.grandviewresearch.com/industry-analysis/digital-health-market
https://www.mckinsey.com/industries/healthcare/our-insights/telehealth-a-quarter-trillion-dollar-post-covid-19-reality
https://journals.plos.org/digitalhealth/article?id=10.1371/journal.pdig.0000198
https://www.nature.com/articles/s41586-019-1799-6
https://www.accenture.com/us-en/insights/health/leaders-make-recent-digital-health-gains-last


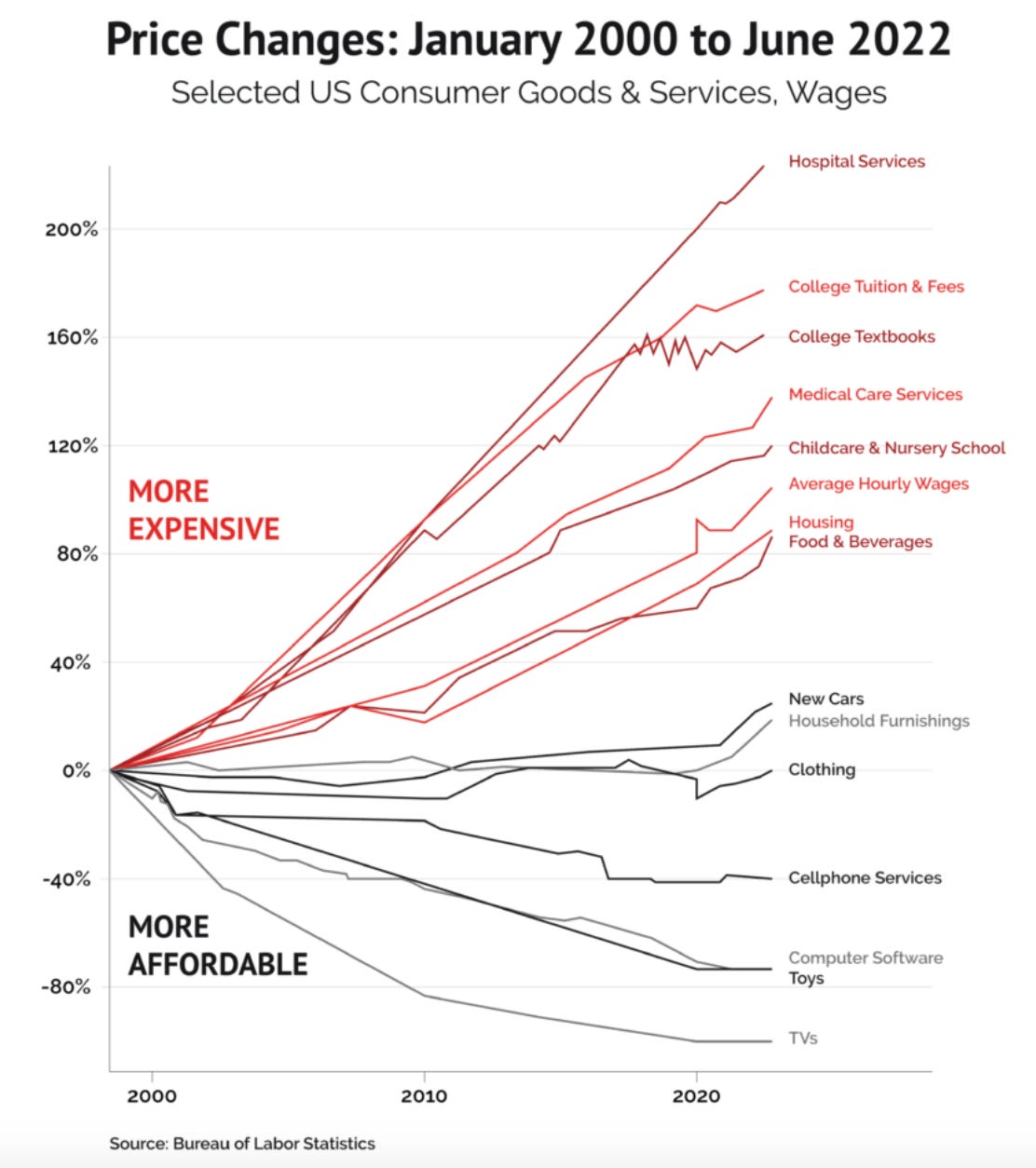

An incredible amount of information in this essay. The chart on medical expenses compared to other consumer expenditures says it all.
I tend to think that AI can have a significant role in general wellness medicine. At my annual physical the first half hour or so consists of reading though the results of the blood test, comparing to prior analyses and reaching conclusions and action steps. Seems to me to be a job that could mostly be done by a "bot" under the supervision of an actual doctor.